Radiation Health Risks
How can we assess impacts of exposures?
The ability to gauge radiation at vanishingly low concentrations gives scientists a powerful tool for understanding ocean processes. “We can measure down to less than 1 becquerel”—one radioactive decay event per second, said Ken Buesseler, a marine chemist at Woods Hole Oceanographic Institution. “But just because we can measure it doesn’t mean it’s necessarily harmful to human health.”
At what point, then, is radiation exposure harmful to humans? And what are the likely health effects of the exposures incurred from Fukushima?
Buesseler and colleagues saw plenty of debris from the tsunami floating in the ocean on a research expedition off the Japanese coast in June 2011, and they continuously monitored radiation levels to ensure that they were not in harm’s way. Measuring seawater samples later in their labs, they showed that the levels of the radioisotope cesium-137 offshore were lower than acceptable levels in drinking water in the United States, yet still more than 1,000 times higher than existed prior to the Fukushima nuclear disaster. And though traces of Fukushima radiation will eventually show up all the way across the Pacific, they will be just that: traces—not enough to affect human health directly.
There is, however, more concern about the Fukushima radioisotopes that end up in fish and seaweed—mainstays of the Japanese diet. “Here we’re talking about accumulation in something you’re going to eat internally versus being exposed to externally,” Buesseler said at the Fukushima and the Ocean conference in Tokyo in November 2012. Monitoring of cesium in fish taken from affected areas continues to show an unexplained persistence of higher-than-pre-disaster levels, and the occasional anomalies of individual fish caught near the power plant that register sky-high numbers. Both are indications that more study is needed, and that fish from the Fukushima region can’t yet be pronounced safe to eat. To date, fisheries remain closed in those areas.
The larger health worries are those to be faced on land. As Buesseler explained, “The difference is, on land, once the radiation falls, it stays put, taken up by soils and plants. So you have a long-term source and higher direct exposure to people that doesn’t exist in the ocean, where the radiation is diluted.”
Fortuitous winds
Fortunately, because of prevailing weather conditions at the time of the accident, 80 percent of the radiation released from the doomed Fukushima Dai-ichi nuclear power plant reactors fell on the ocean. That and evacuation of areas affected on land kept acute human exposures limited. Still, shifting winds and rain a few days after the meltdowns resulted in patchy hot spots of fallout over land.
The highest exposures, not surprisingly, were suffered by workers inside the plant. Over the days of full-bore chaos when emergency crews raced to limit the scope of the disaster, 167 workers received a radiation dose of more than 100 millisieverts, reported the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). One hundred millisieverts is the level above which experts have demonstrated measurable increases in cancer risks. There is still debate about risks for people exposed to lower doses, because these risks are lower and harder to detect.
For an additional 20,000 Tokyo Electric Power Co. workers, and for the roughly 150,000 Japanese citizens living in the fallout zone, exposures were lower. According to the World Health Organization, most of those residents received doses between 2 and 10 millisieverts. In Namie town and Iitate village, two nearby communities where evacuation was delayed, residents received 10 to 50 millisieverts. In one troubling exception, several news reports cited Japanese officials saying that 1-year-olds in Namie town may have been exposed to 100 to 200 millisieverts of radioactive iodine-131.
This radioisotope, with a short-lived half-life of about eight days, may pose the most serious health threat from Fukushima radiation. James Seward, medical director at Lawrence Livermore National Laboratory in California, told conference attendees that different radioisotopes are taken up differently in the human body, and they target different organs. Iodine gathers in the thyroid, and in high enough doses, its presence causes an increased risk of thyroid cancer, particularly in children.
Thyroid cancer has been the single largest health impact of the Chernobyl nuclear disaster, with 6,000 cases identified by 2005, according to an UNSCEAR report. Fortunately, this cancer is usually treatable and results in few fatalities.
As Seward hastened to add, the average exposures in Chernobyl were much higher than those experienced at Fukushima. Government data collected from 1,080 children in Iwate and other nearby prefectures shows that none received a thyroid dose higher than 35 millisieverts. “There is certainly some risk of thyroid cancer in children in this population,” Seward said. “But that risk is very low overall and may be difficult to measure with epidemiologic techniques.”
The low-dose question
But concerns remain about lingering exposures to cesium radioisotopes, for example. Mitsuyoshi Urashima, a pediatric oncologist at Jikei University School of Medicine, has tested pregnant women and children in Kouri town, adjacent to Fukushima City, and found that one in 100 has received a dose higher than worldwide background radioactivity levels. The anxiety is a reflection, at least in part, of prevailing uncertainty about the effects of low-level exposures.
Seward, a practicing physician with a specialty in occupational medicine and experience treating acute radiation poisoning, tackled what is known as the low-dose question. He began by laying out some of the basics.
Humans around the globe are constantly exposed to small amounts of radiation, but at low levels that don’t appear to produce known health effects, Seward said. This background radiation exposure averages 3 millisieverts per year and comes from natural and artificial sources. The former includes cosmic radiation (high-energy particles originating outside Earth’s solar system) and radon in rocks; the latter includes medical X-rays, CT scans, and even travel in airplanes at high altitudes, where the thinner atmosphere offers less protection against incoming cosmic radiation. For the same reason, exposure is higher for people living at high altitudes and can range up to 10 millisieverts a year.
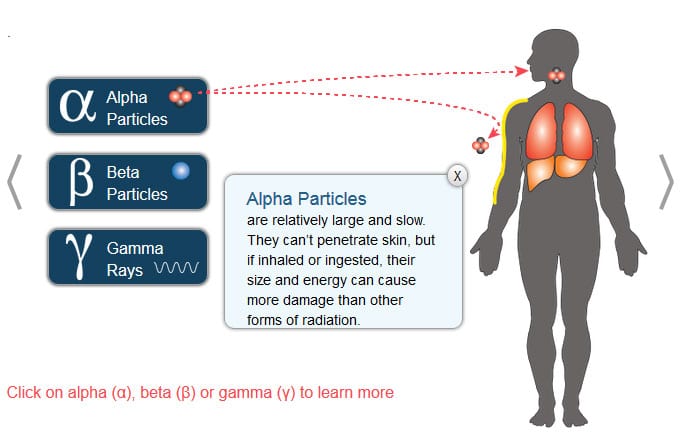
Radiation can enter the body via internal and external pathways. It can penetrate the body like X-rays, and it can be inhaled from the air, absorbed through the skin, and ingested with food and drink. Once within the body’s cells, these unstable radioisotopes act to damage DNA, either directly, by striking DNA or other cellular molecules themselves, or indirectly, by creating free radicals—highly reactive molecules that can cause the damage.
As long as the dose is limited, the body has repair mechanisms to keep this damage in check. When that system is overwhelmed, however, radiation can create two types of effects. The first, called deterministic effects, occurs to any individual who receives high-dose exposures. They produce health problems that include skin burns, eye cataracts, and, in pregnant women, harm to the developing fetus. Thankfully, Seward said, “this type of effect has not turned out to be a significant issue around Fukushima, and it does not appear that even the more highly exposed nuclear plant workers experienced these health problems.”
Random effects
The other type of effects are called stochastic or random, and most significantly, they include cancer. A lot of what we know about stochastic effects in humans, Seward said, comes from long-term studies of the survivors of the atomic bombs dropped on Hiroshima and Nagasaki. These studies show that above doses of 100 millisieverts, the risk of getting cancer—but not the severity of the disease—rises in a straight line with exposure.
At 100 millisieverts, the increased risk of cancers is very small: around 0.5 percent, he noted. As he explained it, the average Japanese male, throughout his lifetime, has a 26 percent chance of developing a fatal cancer from any cause; the average female, 16 percent. With the addition of a 100-millisievert radiation exposure, that risk rises to about 26.5 and 16.5 percent, respectively. For individuals exposed as children, the numbers are slightly higher.
Below that 100-millisievert level, however, the picture becomes much less clear. “There is only limited evidence to show a dose-related effect,” Seward said. Safety standards established for these low-level exposures—for power plant workers, for instance, and radiation technicians—depend therefore on something called the linear no-threshold model, which, as Seward noted, is simply extrapolated from the impacts seen at higher doses. In essence, the model conservatively holds that any dose of radiation increases cancer risk: There is no bottom threshold.
The hitch is that scientists by no means agree on the validity of this theory. Some say low-dose exposures below some threshold are harmless. Some even claim they have a beneficial effect on DNA repair (a phenomenon known as hormesis). Others argue that low-dose risks may be higher than currently predicted.
“The key point,” Seward said, “is that the linear no-threshold model is best applied for setting safety standards.” It errs on what many scientists consider to be the safe side. It is unlikely to be an accurate predictor of the numbers of cancers resulting from exposures when very low doses are involved.
The challenge, Seward said, is that in a population where radiation exposures are very low, it may be difficult to detect a significant change in cancer rates and attribute that with certainty to the Fukushima releases.
Confounding factors
In July 2012, uncertainties notwithstanding, Stanford University scientists John Ten Hoeve and Mark Jacobson published a prediction of the total cancer casualties that will eventually accrue from the Fukushima nuclear disaster: 130 deaths and 180 additional cancers, they say. Ten Hoeve and Jacobson pointed out that, while evacuation of the affected precincts was necessary under the circumstances, more individuals may have died in the process of that evacuation than are expected to die from the long-term effects of radiation exposure.
The study, published in the journal Energy and Environmental Studies, was widely reported in Japan and elsewhere. As Seward noted, however, its results encompass a vast range of possibilities: between 15 and 1,100 fatalities and between 24 and 1,800 additional cancers.
“To most people, there’s a big difference between 39 cancers and 2,900,” wrote Geoff Brumfiel, a journalist who covered the Fukushima crisis for the journal Nature and who attended the conference. “The problem is that these types of estimate depend on models and assumptions.”
“It’s a challenging problem,” said Dale Preston, a biostatistician at Hirosoft International in Eureka, Calif., who specializes in radiation health effects. “One of the main reasons is that radiation-affected cases are indistinguishable from other cases. It requires very well-designed epidemiological studies to estimate the number of affected cases, and in the case of low doses, it requires very large studies that go on for a long period of time.”
The reality is that the estimated increases in fatalities and cancers are small compared with the overall cancer mortality in Japan and elsewhere, which affects 15 to 25 percent of the total population.
“We do know that the magnitude of effect depends on the dose,” Preston continued. “We also know that the effects, if any, of low to moderate doses appear to be small.” But sifting out those effects requires accounting for how they will vary—not just with dose rate but with factors such as time since exposure, age at exposure, sex, and ethnicity, not to mention interactions with other risk factors like smoking. Despite these challenges, he argued, some data that are relevant to Fukushima do exist.
He pointed first to the A-bomb survivors. Among 93,000 who were exposed to radiation at Hiroshima and Nagasaki, he said, 25 percent received doses within the low-dose range. A second long-term study involves some 30,000 villagers in the Techa River valley of southern Russia, whose exposure was quite different: repeated environmental releases from a plutonium production facility during the 1950s. Both studies, Preston said, show slightly increased rates of leukemia and other cancers associated with exposures below 100 millisieverts.
Long-term health impact studies needed
In February 2013, the World Health Organization issued a health risk assessment report on the Fukushima nuclear accident conducted by more than two dozen scientists in various fields. It estimated somewhat elevated risk for cancers in certain age and sex groups in the most contaminated areas—for example, for girls exposed as infants to radioactivity in the most affected regions of Fukushima Prefecture—but no observable increase in cancer rates in wider Japanese populations and no discernible health risks outside Japan.
But, the report concluded, “This health risk assessment is based on the current state of scientific knowledge. … Because scientific understanding of radiation effects, particularly at low doses, may increase in the future, it is possible that further investigation may change our understanding of the risks of this radiation accident.”
Questions and concerns also linger about exposures from short-lived radioactive gases released from the plant, such as the noble gas xenon-133, which has a half-life of five days. Several speakers raised this issue at a conference on the medical and ecological consequences of Fukushima at the New York Academy of Medicine in March 2013, said Buesseler, who attended that conference on the two-year anniversary of the disaster.
Preston and Seward agreed on the importance of a long-term study of the Fukushima population—even “if the power to detect effects may be limited,” Preston said. “If the study finds nothing, that in itself will be reassuring to the public.”
In July the Fukushima Medical University launched an ambitious survey intended to establish individual radiation exposures by pinpointing people’s exact whereabouts during the crisis, the amount of time they spent outdoors, and everything they ate and drank. The study will provide ongoing thyroid exams for all of Fukushima prefecture’s children, and checkups for pregnant women and evacuees. It is expected to continue for at least 30 years.
Preston and Seward both suggested including another component to long-term health studies on Fukushima: a careful analysis of the disaster’s psychological impacts. In the end, they said, the stress of living with the uncertainty about exposure to low-dose radiation, which science cannot yet unravel, may well turn out to be the largest and longest-lived health effect of all.
Related links:
The Accidents at Fukushima
http://www.whoi.edu/website/fukushima-symposium/overview
Fukushima and the Ocean Colloquium, May 9, 2013
http://www.whoi.edu/main/morss/fukushima
Fukushima Radiation the Pacific
https://www.whoi.edu/page.do?pid=67796
Lessons from the Japan Earthquake
http://www.whoi.edu/oceanus/viewArticle.do?id=131749
Café Thorium (Ken Buesseler’s Lab)
http://cafethorium.whoi.edu/website/about/index.html
WHOI Tsunami website
http://www.whoi.edu/home/interactive/tsunami/indexEnglish.html
Fishing for Answers off Fukushima
https://www.whoi.edu/press-room/news-release/fukushima-fish/
Radiation and the Oceans
http://www.whoi.edu/page.do?pid=83397&tid=3622&cid=94989
Japan, 2011
http://www.whoi.edu/main/japan-2011